Keywords
Abstract
Magnetic resonance imaging (MRI)-targeted transperineal prostate biopsy allows a more precise sampling of suggestive lesions. We describe a series of 10 cases for MRI-targeted transperineal prostate biopsy, of which 8 were successfully performed under ultrasound-guided caudal epidural anaesthesia. With the appropriate local anaesthetic volume and concentration, caudal epidural provides ideal conditions for this day case procedure.
References
Hung S, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660
Jemal A, Fedewa SA, Ma J, et al. Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. JAMA. 2015;314(19):2054–2061. https://doi.org/10.1001/jama.2015.14905
Aus G, Damber J-E, Hugosson J. Prostate biopsy and anaesthesia: an overview. Scand J Urol Nephrol. 2005;39(2):124–9. https://doi.org/10.1080/00365590510007784
Drost F-JH, Osses DF, Nieboer D, et al. Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst Rev. 2019;4:CD012663. https://doi.org/10.1002/14651858.CD012663.pub2
Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378(19):1767–77. https://doi.org/10.1056/NEJMoa1801993
Ahdoot M, Wilbur AR, Reese SE, et al. MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis. N Engl J Med. 2020;382(10):917–28. https://doi.org/10.1056/NEJMoa1910038
Luscombe CJ, Cooke PW. Pain during prostate biopsy. Lancet. 2004;363(9424):1840–1. https://doi.org/10.1016/S0140-6736(04)16392-7
Wade J, Rosario DJ, Macefield RC, et al. Psychological impact of prostate biopsy: Physical symptoms, anxiety, and depression. J Clin Oncol. 2013;31(33):4235–41. https://doi.org/10.1200/JCO.2012.45.4801
Maccagnano C, Scattoni V, Roscigno M, et al. Anaesthesia in transrectal prostate biopsy: which is themost effective technique? Urol Int. 2011;87:1–13. https://doi.org/10.1159/000327827
Practice guidelines for moderate procedural sedation and analgesia 2018: A report by the American society of anesthesiologists task force on moderate procedural sedation and analgesia, the American association of oral and maxillofacial surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology. 2018;128(3):437–79. https://doi.org/10.1097/ALN.0000000000002043
Rattenberry W, Hertling A, Erskine R. Spinal anaesthesia for ambulatory surgery. BJA Educ. 2019 Oct;19(10):321-328. https://doi.org/10.1016/j.bjae.2019.06.001
Wang N, Fu Y, Ma H, Wang J, Gao Y. Advantages of caudal block over intrarectal local anesthesia plus periprostatic nerve block for transrectal ultrasound guided prostate biopsy. Pak J Med Sci Q. 2016;32(4):978–82. https://doi.org/10.12669/pjms.324.9823
Kaur J, Singh P. Pudendal Nerve Entrapment Syndrome. StatPearls Treasure Island (FL); 2021.
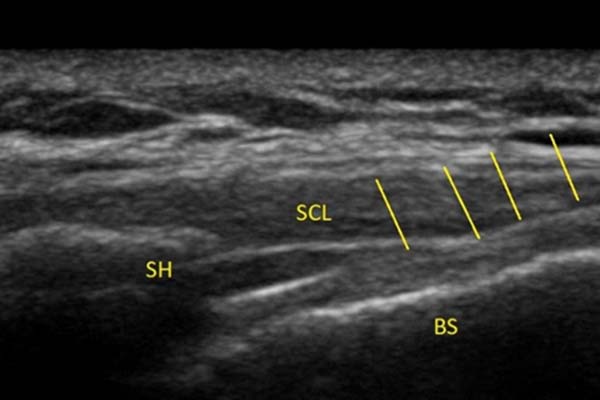
Kim YH, Park HJ, Cho S, Moon DE. Assessment of factors affecting the difficulty of caudal epidural injections in adults using ultrasound. Pain Res Manag. 2014 Sep-Oct;19(5):275-9. https://doi.org/10.1155/2014/679128
Chen CP, Tang SF, Hsu TC, et al. Ultrasound guidance in caudal epidural needle placement. Anesthesiology. 2004;101:181–4. https://doi.org/10.1097/00000542-200407000-00028