Keywords
Abstract
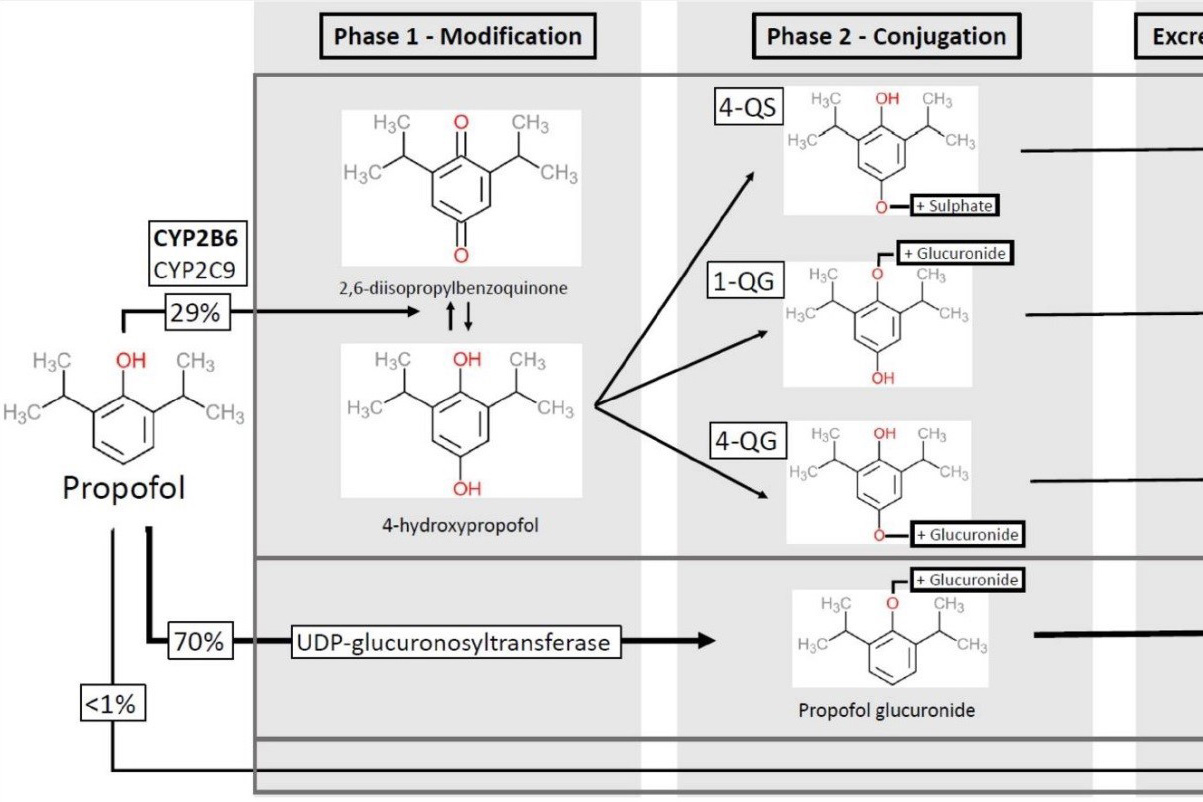
Although propofol is a commonly used medication for inducing general anaesthesia, it is not without side effects. In this case report, we present a patient with hepatocellular carcinoma who experienced postoperative unconsciousness following general anaesthesia induction using propofol. While this is a rare occurrence, it underscores the importance of remaining vigilant and understanding propofol’s pharmacokinetic properties. The drug can be redistributed from fat tissues into the systemic circulation, resulting in delayed recovery and potential adverse effects. We also discuss the possible impact of disease interactions, particularly hepatic impairment with possible CYP450 deficiency, on propofol metabolism. We stress the necessity of closely monitoring patients during anaesthesia induction and maintenance.
References
MIMS Online Team. Fresofol 1% MCT/LCT Full Prescribing Information, Dosage & Side Effects | MIMS Hong Kong. MIMS Hong Kong [Internet]. n.d. Available from: https://www.mims.com/hongkong/drug/info/fresofol%201percent%20mct-lct?type=full
Suh SJ, Yim HJ, Yoon EL, et al. Is propofol safe when administered to cirrhotic patients during sedative endoscopy? Korean J Intern Med. 2014;29(1):57. https://doi.org/10.3904/kjim.2014.29.1.57
Sahinovic MM, Struys MM, Absalom AR. Clinical pharmacokinetics and pharmacodynamics of propofol. Clin Pharmacokinet. 2018;57(12):1539-1558. https://doi.org/10.1007/s40262-018-0672-3
Iwersen-Bergmann S, Rösner P, Kühnau HC, Junge M, Schmoldt A. Death after excessive propofol abuse. Int J Legal Med. 2001;114:248-251. https://doi.org/10.1007/s004149900129
Propofol - LiverTox - NCBI Bookshelf. Propofol - LiverTox - NCBI Bookshelf. 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547909/#:~:text=Propofol%20has%20been%20associated%20with,an%20enlarged%20or%20fatty%20liver
Bosetti C, Turati F, La Vecchia C. Hepatocellular carcinoma epidemiology. Best Pract Res Clin Gastroenterol. 2014;28(5):753-70. https://doi.org/10.1016/j.bpg.2014.08.007
Chen X, Liu HP, Li M, Qiao L. Advances in non-surgical management of primary liver cancer. World J Gastroenterol. 2014;20(44):16630. https://doi.org/10.3748/wjg.v20.i44.16630
Yan T, Lu L, Xie C, et al. Severely impaired and dysregulated cytochrome P450 expression and activities in hepatocellular carcinoma: implications for personalized treatment in patients severely impaired and dysregulated activities of CYPs in HCC. Mol Cancer Ther. 2015;14(12):2874-2886. https://doi.org/10.1158/1535-7163.MCT-15-0274
Vanlander AV, Menten B, Smet J, et al. Possible pathogenic mechanism of propofol infusion syndrome involves coenzyme Q. Anesthesiology. 2015;122(2):343-352. https://doi.org/10.1097/ALN.0000000000000484
Hemphill S, McMenamin L, Bellamy MC, Hopkins PM. Propofol infusion syndrome: a structured literature review and analysis of published case reports. Br J Anaesth. 2019;122(4):448-459. https://doi.org/10.1016/j.bja.2018.12.025