Keywords
Abstract
Introduction: Multimodal analgesia regime in enhanced recovery after surgery (ERAS) protocol is associated with fewer perioperative complications, shorter hospital stays, and reduced opioid dependence. Although ERAS strategies have been widely accepted and implemented in current practice, there is limited data regarding its application and outcomes in the Malaysian population, particularly in colorectal surgeries. Hence, this study was conducted to examine postoperative pain scores after implementing a multimodal analgesia regime as per ERAS anaesthesia protocol.
Methods: This is a retrospective study using data collection forms. Data were collected from the case notes of patients who underwent colorectal surgery complying with the ERAS anaesthesia protocol from January 2022 to December 2023. Pain score was assessed when the patient arrived at recovery bay, subsequently reassessed at 2 hours postoperative, 6 hours postoperative, 12 hours postoperative, 1 day postoperative, and finally on postoperative day 2.
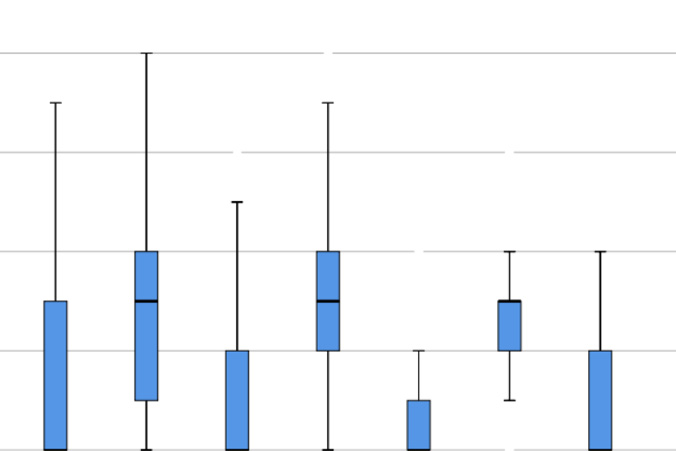
Results: A total of 139 samples were recruited in this retrospective study. The median postoperative pain scores at rest were consistently 0 from arrival at recovery bay to postoperative day 2. On the other hand, the median pain score upon movement was 1 (range 0–3) when patients reached the recovery bay, and persistently 3 during
postoperative 2 hours, 6 hours, and 12 hours, after which the median pain score upon movement became 2 on postoperative day 1 and day 2.
Conclusions: Multimodal analgesia in line with the ERAS protocol in colorectal surgeries is feasible, safe and efficient.
References
Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: 2018. World J Surg. 2019; 43: 659-695. https://doi.org/10.1007/s00268-018-4844-y
Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534-540. https://doi.org/10.1213/01.ANE.0000068822.10113.9E
Soffin EM, Lee BH, Kumar KK, Wu CL. The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth. 2019 Jun;122(6):e198-e208. https://doi.org/10.1016/j.bja.2018.11.019
Jih Huei T, Kumar N, Tan Chor Lip H et al. Outcome of ERAS in colorectal cancer surgery. Chron. 2022;27:133-135.
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011; 146:571-577. https://doi.org/10.1001/archsurg.2010.309
Kranke P, Jokinen J, Pace NL, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev 2015; 2015. https://doi.org/10.1002/14651858.CD009642.pub2
Foo I, Macfarlane AJR, Srivastava D, et al. The use of intravenous lidocaine for postoperative pain and recovery: international consensus statement on efficacy and safety. Anaesthesia. 2021;76:238-250. https://doi.org/10.1111/anae.15270
Simpson JC, Bao X, Agarwala A. Pain Management in Enhanced Recovery after Surgery (ERAS) Protocols. Clin Colon Rectal Surg. 2019 Mar;32(2):121-128. https://doi.org/10.1055/s-0038-1676477
Kim SH, Stoicea N, Soghomonyan S, Bergese SD. Intraoperative use of remifentanil and opioid induced hyperalgesia/acute opioid tolerance: Systematic review. Front Pharmacol. 2014;5 May:1-9. https://doi.org/10.3389/fphar.2014.00108
Baidya DK, Khanna P, Maitra S. Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: A systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2014;18: 626-636. https://doi.org/10.1093/icvts/ivt551
Manassero A, Bossolasco M, Carrega M, Coletta G. Postoperative thoracic epidural analgesia: Adverse events from a single-center series of 3126 patients. Local Reg Anesth. 2020;13:111-119. https://doi.org/10.2147/LRA.S272410
Paladini G, Carlo S Di, Musella G, et al. Continuous wound infiltration of local anesthetics in postoperative pain management: Safety, efficacy and current perspectives. J Pain Res. 2020; 13: 285-294. https://doi.org/10.2147/JPR.S211234
Ventham NT, Hughes M, O’Neill S, Johns N, Brady RR, Wigmore SJ. Systematic review and meta-analysis of continuous local anaesthetic wound infiltration versus epidural analgesia for postoperative pain following abdominal surgery. Br J Surg. 2013;100:1280-1289. https://doi.org/10.1002/bjs.9204
Dong Y, Zhang Y, Jin C. Comprehensive economic evaluation of enhanced recovery after surgery in hepatectomy. Int J Equity Health. 2021;20:1-9. https://doi.org/10.1186/s12939-021-01583-3