Keywords
Abstract
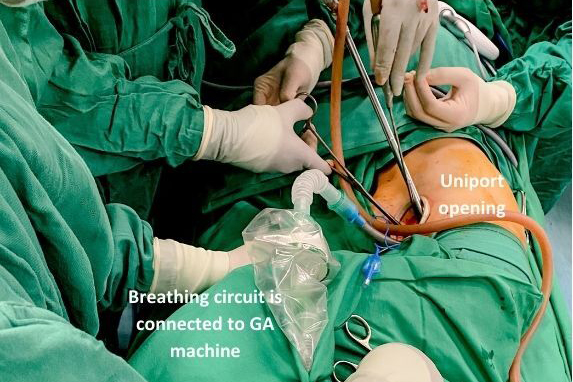
The occurrence of contralateral pneumothorax during non-intubated video-assisted thoracoscopic surgery (NiVATS) is rare and difficult to diagnose intraoperatively due to its non-specific clinical presentations. Temporary desaturation is not uncommon in NiVATS. This report highlights a case where maintaining oxygenation proved challenging despite various remedial interventions, ranging from use of high-flow oxygen delivery to manual jet ventilation via Cook airway exchange catheter during right NiVATS for distal tracheal mass resection and reconstruction. Intermittent cross-field ventilation was employed during tumour removal and tracheal anastomosis to maintain oxygenation. Postoperative chest X-ray revealed the reason for oxygenation failure: pneumothorax on the left side. The left-side chest tube was not inserted because the patient remained asymptomatic post-extubation. The patient was discharged well on postoperative day 8. Repeated bronchoscopy at 1-month post-surgery revealed intact anastomosis. Prompt diagnosis of pneumothorax in high-risk surgeries and contingency airway plans are imperative in managing patients undergoing NiVATS to prevent airway mishaps.
References
Liang H, Gonzalez-Rivas D, Zhou Y, et al. Nonintubated Anesthesia for Tracheal/Carinal Resection and Reconstruction. Thorac Surg Clin. 2020 Feb;30(1):83-90. https://doi.org/10.1016/j.thorsurg.2019.08.007
Cheng YJ. Role, benefits and limitations of non-intubated anesthesia in thoracic surgery. Video-Assisted Thoracic Surgery. 2017 Sep 13;2(9).
Koh LY, Hwang NC. Anesthesia for nonintubated video-assisted thoracoscopic surgery. J Cardiothorac Vasc Anesth. 2023 Jul;37(7):1275-1283. https://doi.org/10.1053/j.jvca.2023.02.048
Dharmaraj B, Sathiamurthy N, Balasubbiah N, Kamil AN. Non-intubated video-assisted thoracoscopic tracheal resection and reconstruction for benign distal tracheal stenosis—a case report and review of literature. AME Surgical Journal. 2021 Dec 30;1.
Balasubbiah N, Sathiamurthy N, Dharmaraj B, et al. Tracheal resection and reconstruction: A 3-year case series of 14 patients. Med J Malaysia. 2022 Sep 1;77(5):623.
Rosboch GL, Lyberis P, Ceraolo E, et al. The anesthesiologist’s perspective regarding non-intubated thoracic surgery: a scoping review. Front Surg. 2022 Apr 4;9:868287. https://doi.org/10.3389/fsurg.2022.868287
Kumata S, Matsuoka K, Nagai S, Ueda M, Okada Y, Miyamoto Y. Contralateral tension pneumothorax during video-assisted thoracic surgery for lung cancer in a patient with obesity and rib fractures: a case report and review of the literature. J Med Case Rep. 2020 Dec;14:1-4. https://doi.org/10.1186/s13256-020-02556-w
Choy MC, Pescod D. Pneumothorax in association with spontaneous ventilation general anaesthesia--an unusual cause of hypoxaemia. Anaesth Intensive Care. 2007 Apr;35(2):270-3. https://doi.org/10.1177/0310057X0703500218
Malik S, Shapiro WA, Jablons D, Katz JA. Contralateral tension pneumothorax during one-lung ventilation for lobectomy: diagnosis aided by fiberoptic bronchoscopy. Anesth Analg. 2002 Sep;95(3):570-2, table of contents. https://doi.org/10.1097/00000539-200209000-00014