Keywords
Abstract
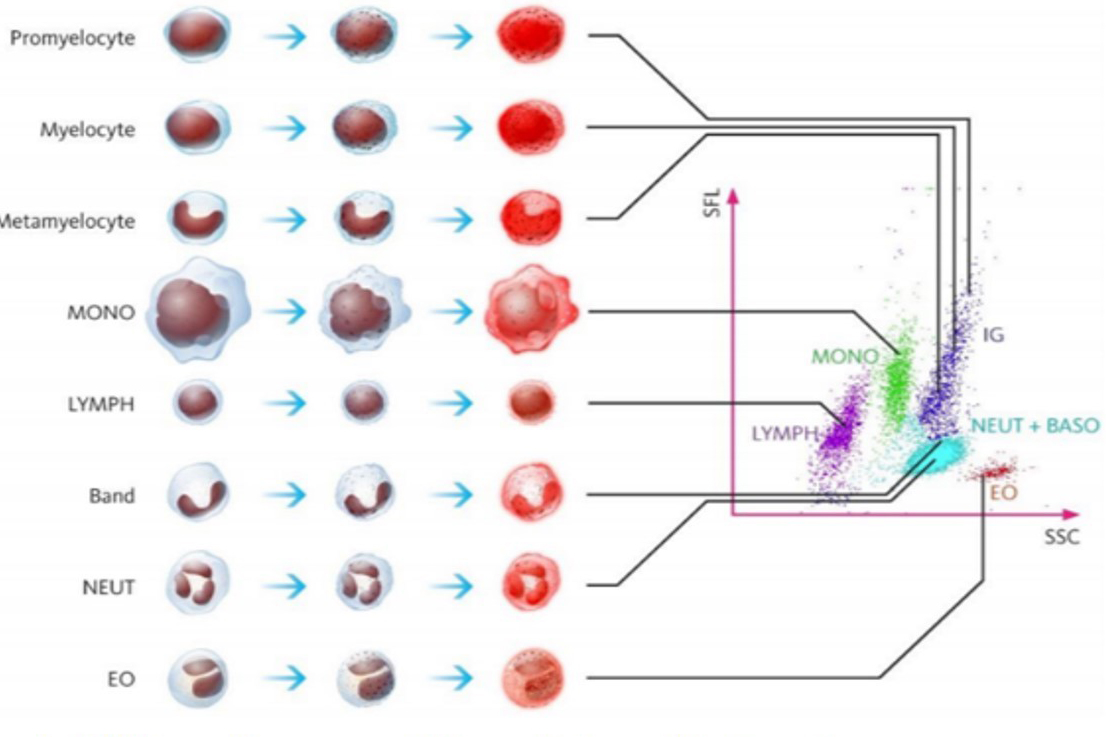
The full blood count is one of the simplest and most ordered blood investigations in daily practice. Its use and that of other classic markers for iron deficiency have been well established. Recently, there has been increased attention to the potential for fluorescence flow cytometry as an enhancement to the classic blood count. This paper explores the potential of new cellular biomarkers using this technology to enhance our diagnosis of iron deficiency anaemia (IDA) and differentiate between sepsis and systemic inflammation. For IDA, parameters such as the reticulocyte haemoglobin equivalent (RET-He) and the difference between reticulocyte and erythrocyte haemoglobin equivalent (DELTA-He) are exciting additions to enhance the speed and accuracy of its diagnosis. RET-He, which is defined as the haemoglobin content in reticulocytes, offers a more immediate reflection of iron availability for erythropoiesis compared to traditional markers such Hb concentration and mean corpuscular volume. The integration of advanced technologies, such as fluorescence flow cytometry, into routine blood counts can significantly improve diagnostic precision, allowing for a more nuanced understanding of the haematopoietic system and immune response. In critically ill patients, these new parameters can help to differentiate between various inflammatory responses and infections, providing valuable insights into the activation status of neutrophils and other immune cells. Parameters such as immature granulocytes and neutrophil reactivity intensity have shown promise in discriminating between systemic inflammatory response syndrome and sepsis. The introduction of these markers holds the potential for quicker and more cost-effective assessments for sepsis. The addition of fluorescence flow cytometry parameters to our armament of investigations for blood counts could enhance our abilities to practice precision medicine.
References
Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care. 2010;14(1):R15. https://doi.org/10.1186/cc8872
Pekelharing J, Hauss O, De R, et al. Haematology Reference Intervals for Established and Novel Parameters in Healthy Adults. Diagnostic Perspectives. 2010;1.
Haematology S. SYSMEX EDUCATIONAL ENHANCEMENT AND DEVELOPMENT | DECEMBER 2015. 2016.
Nemeth E, Ganz T. The role of hepcidin in iron metabolism. Acta Haematol. 2009;122(2-3):78-86. https://doi.org/10.1159/000243791
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. 2011. https://www.who.int/publications/i/item/WHO-NMH-NHD-MNM-11.1
Meybohm P, Choorapoikayil S, Zacharowski K. Patient Blood Management in der Intensivmedizin. Intensivmedizin up2date. 2017;13(03):291-307. https://doi.org/10.1055/s-0043-110651
World Health Organization. The urgent need to implement patient blood management: policy brief. 2021. https://www.who.int/publications/i/item/9789240035744
Muñoz M, Acheson AG, Bisbe E, et al. An international consensus statement on the management of postoperative anaemia after major surgical procedures. Anaesthesia. 2018;73(11):1418-1431. https://doi.org/10.1111/anae.14358
Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832-1843. https://doi.org/10.1056/NEJMra1401038
Almashjary MN, Barefah AS, Bahashwan S, et al. Reticulocyte Hemoglobin-Equivalent Potentially Detects, Diagnoses and Discriminates between Stages of Iron Deficiency with High Sensitivity and Specificity. J Clin Med. 2022;11(19). https://doi.org/10.3390/jcm11195675
Park SH, Park CJ, Lee BR, et al. Sepsis affects most routine and cell population data (CPD) obtained using the Sysmex XN-2000 blood cell analyzer: neutrophil-related CPD NE-SFL and NE-WY provide useful information for detecting sepsis. Int J Lab Hematol. 2015;37(2):190-198. https://doi.org/10.1111/ijlh.12261
Hönemann C, Hagemann O, Doll D, Luedi MML, Ruebsam ML, Meybohm P. [Reticulocyte hemoglobin equivalent as a diagnostic marker for the current iron deficiency : Old wine in new bottles]. Anaesthesist. 2020;69(12):919-925. https://doi.org/10.1007/s00101-020-00870-y
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Jama. 2016;315(8):801-810. https://doi.org/10.1001/jama.2016.0287
Cornet E, Boubaya M, Troussard X. Contribution of the new XN-1000 parameters NEUT-RI and NEUT-WY for managing patients with immature granulocytes. Int J Lab Hematol. 2015;37(5):e123-126. https://doi.org/10.1111/ijlh.12372
Urrechaga E BO, Aguirre U, García S, Pulido E. Neutrophil Cell Population Data Biomarkers for Acute Bacterial Infection. . J Pathol Infect. 2018;1(1):1-7. https://asclepiusopen.com/journal-of-pathology-and-infectious-diseases/volume-1-issue-1/6.pdf
Stiel L, Delabranche X, Galoisy AC, et al. Neutrophil Fluorescence: A New Indicator of Cell Activation During Septic Shock-Induced Disseminated Intravascular Coagulation. Crit Care Med. 2016;44(11):e1132-e1136. https://doi.org/10.1097/ccm.0000000000001851
Ayres LS, Sgnaolin V, Munhoz TP. Immature granulocytes index as early marker of sepsis. Int J Lab Hematol. 2019;41(3):392-396. https://doi.org/10.1111/ijlh.12990
Nierhaus A, Klatte S, Linssen J, et al. Revisiting the white blood cell count: immature granulocytes count as a diagnostic marker to discriminate between SIRS and sepsis--a prospective, observational study. BMC Immunol. 2013;14:8. https://doi.org/10.1186/1471-2172-14-8
Linssen J, Ermens A, Berrevoets M, et al. A novel haemocytometric COVID-19 prognostic score developed and validated in an observational multicentre European hospital-based study. Elife. 2020;9. https://doi.org/10.7554/eLife.63195
Weimann K, Zimmermann M, Spies CD, et al. Intensive Care Infection Score--A new approach to distinguish between infectious and noninfectious processes in intensive care and medicosurgical patients. J Int Med Res. 2015;43(3):435-451. https://doi.org/10.1177/0300060514557711
Froessler B, Palm P, Weber I, Hodyl NA, Singh R, Murphy EM. The Important Role for Intravenous Iron in Perioperative Patient Blood Management in Major Abdominal Surgery: A Randomized Controlled Trial. Ann Surg. 2016;264(1):41-46. https://doi.org/10.1097/sla.0000000000001646