Keywords
Abstract
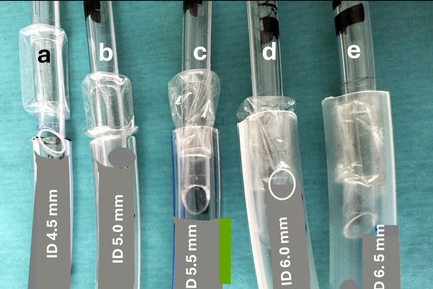
This review critically analyses literature on the anatomy of the paediatric larynx published from 1897 to 2024, with an emphasis on key studies by Fayoux et al. and Isa et al. These pivotal investigations highlighted significant misconceptions and gaps in knowledge concerning the use of cuffed endotracheal tubes (ETTs) in infants and young children. Despite a comprehensive body of research spanning over a century, essential findings related to laryngeal dimensions and injury mechanisms during intubation were often overlooked or misrepresented in both historical and modern publications. Isa et al. conducted a detailed anatomical study using fresh paediatric larynges from autopsies, comparing their results to prior landmark research. Their methods included placing cuffless ETTs and Microcuff tubes (MCTs) in the laryngeal lumen and measuring the placement at the vocal cord level. The study demonstrated that the cricoid outlet (CO) is a rigid, circular structure—the narrowest part of the paediatric airway—and that it remains less distensible than the glottis or trachea. Fayoux et al.’s earlier work with 150 neonatal specimens confirmed this rigidity and emphasised the potential for significant airway damage when oversized ETTs are forced through the CO. This review highlights that radiological and endoscopic approaches often fail to accurately represent paediatric laryngeal anatomy, leading to clinical practices where inappropriate tube sizes are used. MCTs, despite their popularity, were shown to exceed CO dimensions in infants, risking mucosal damage and scarring. The failure to adopt these anatomical insights into clinical guidelines has led to practices that may compromise patient safety, such as using MCTs in premature infants where the deflated cuff’s outer diameter (OD) exceeds CO diameters. Key measurements from Isa et al. reaffirm that cuffless ETTs based on ODs, rather than internal diameters, are more appropriate for the paediatric airway. This review urges the inclusion of accurate anatomical data, such as the findings of Fayoux et al. and Isa et al., into clinical protocols to prevent airway trauma and improve paediatric intubation outcomes.
References
Fayoux P, Devisme L, Merrot O, Marciniak B. Determination of endotracheal tube size in a perinatal population: an anatomical and experimental study. Anesthesiology. 2006;104(5):954-960. https://doi.org/10.1097/00000542-200605000-00011
Isa M, Holzki J, Hagemeier A, Rothschild MA, Coté CJ. Anatomical In Vitro Investigations of the Pediatric Larynx: A Call for Manufacturer Redesign of Tracheal Tube Cuff Location and Perhaps a Call to Reconsider the Use of Uncuffed Tracheal Tubes. Anesth Analg. 2021;133(4):894-902. https://doi.org/10.1213/ane.0000000000005565
Holzki J, Brown KA, Carroll RG, Coté CJ. The anatomy of the pediatric airway: Has our knowledge changed in 120 years? A review of historic and recent investigations of the anatomy of the pediatric larynx. Paediatr Anaesth. 2018;28(1):13-22. https://doi.org/10.1111/pan.13281
Bayeux MR. Tubage du larynx dans le Croup. Auto-Extubation. La presse médicale. 1897;6:29-33.
Peter K. Handbuch der Anatomie des Kindes (Handbook of the anatomy of the child). Peter K, Wetzel G, Helderich F, editors. Berlin: Springer; 1936.
Hoeve LJ, Berkovits RN, Eskici O, Verwoerd CD. Acquired laryngeal stenosis in infants and children treated by laryngofissure and stenting. Int J Pediatr Otorhinolaryngol. 1996;35(3):251-261. https://doi.org/10.1016/0165-5876(95)01317-2
Holzki J, Laschat M, Puder C. Iatrogenic damage to the pediatric airway. Mechanisms and scar development. Paediatr Anaesth. 2009;19 Suppl 1:131-146. https://doi.org/10.1111/j.1460-9592.2009.03003.x
Holzki J, Laschat M, Puder C. Stridor is not a scientifically valid outcome measure for assessing airway injury. Paediatr Anaesth. 2009;19 Suppl 1:180-197. https://doi.org/10.1111/j.1460-9592.2009.03004.x
Thomas RE, Rao SC, Minutillo C, Hullett B, Bulsara MK. Cuffed endotracheal tubes in infants less than 3 kg: A retrospective cohort study. Paediatr Anaesth. 2018;28(3):204-209. https://doi.org/10.1111/pan.13311
Zander D, Grass B, Weiss M, Buehler PK, Schmitz A. Cuffed endotracheal tubes in neonates and infants of less than 3 kg body weight-A retrospective audit. Paediatr Anaesth. 2021;31(5):604-610. https://doi.org/10.1111/pan.14104
Williams ZC, Kim SS, Naguib A, Shafy SZ, Tobias JD. Use of cuffed endotracheal tubes in infants less than 5 kilograms: A retrospective cohort study. J Pediatr Surg. 2022;57(3):375-381. https://doi.org/10.1016/j.jpedsurg.2021.02.064
Kim JH, Ahn JH, Chae YJ. Pediatric Application of Cuffed Endotracheal Tube. West J Emerg Med. 2023;24(3):579-587. https://doi.org/10.5811/westjem.59560
Sarhan K, Walaa R, Hasanin A, et al. Cuffed versus uncuffed endotracheal tubes in neonates undergoing noncardiac surgeries: A randomized controlled trial. Pediatric Anesthesia. 2024;34(10):1045-1052. https://doi.org/https://doi.org/10.1111/pan.14953
Salgo B, Schmitz A, Henze G, et al. Evaluation of a new recommendation for improved cuffed tracheal tube size selection in infants and small children. Acta Anaesthesiol Scand. 2006;50(5):557-561. https://doi.org/10.1111/j.1399-6576.2006.01003.x
Tobias JD. Pediatric airway anatomy may not be what we thought: implications for clinical practice and the use of cuffed endotracheal tubes. Paediatr Anaesth. 2015;25(1):9-19. https://doi.org/10.1111/pan.12528
Fayoux P, Marciniak B, Devisme L, Storme L. Prenatal and early postnatal morphogenesis and growth of human laryngotracheal structures. J Anat. 2008;213(2):86-92. https://doi.org/10.1111/j.1469-7580.2008.00935.x
De Orange FA, Andrade RG, Lemos A, Borges PS, Figueiroa JN, Kovatsis PG. Cuffed versus uncuffed endotracheal tubes for general anaesthesia in children aged eight years and under. Cochrane Database Syst Rev. 2017;11(11):Cd011954. https://doi.org/10.1002/14651858.CD011954.pub2
Eckenhoff JE. Some anatomic considerations of the infant larynx influencing endotracheal anesthesia. Anesthesiology. 1951;12(4):401-410. https://doi.org/10.1097/00000542-195107000-00001
Wiel E, Vilette B, Darras JA, Scherpereel P, Leclerc F. Laryngotracheal stenosis in children after intubation. Report of five cases. Paediatr Anaesth. 1997;7(5):415-419. https://doi.org/10.1046/j.1460-9592.1997.d01-101.x
Holzki J. [Tubes with cuffs in newborn and young children are a risk! Remarks on the paper by T. Erb and F. J. Frei (Anaesthesist (2001) 50:395-400]. Anaesthesist. 2002;51(4):321-323; author reply 325-326. https://doi.org/10.1007/s00101-002-0309-6
Sirisopana M, Saint-Martin C, Wang NN, Manoukian J, Nguyen LH, Brown KA. Novel measurements of the length of the subglottic airway in infants and young children. Anesth Analg. 2013;117(2):462-470. https://doi.org/10.1213/ANE.0b013e3182991d42
Wani TM, Rafiq M, Akhter N, AlGhamdi FS, Tobias JD. Upper airway in infants-a computed tomography- based analysis. Paediatr Anaesth. 2017;27(5):501-505. https://doi.org/10.1111/pan.13126
Eckel HE, Koebke J, Sittel C, Sprinzl GM, Pototschnig C, Stennert E. Morphology of the human larynx during the first five years of life studied on whole organ serial sections. Ann Otol Rhinol Laryngol. 1999;108(3):232-238. https://doi.org/10.1177/000348949910800303
Khine HH, Corddry DH, Kettrick RG, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997;86(3):627-631; discussion 627A. https://doi.org/10.1097/00000542-199703000-00015
Litman RS, Weissend EE, Shibata D, Westesson PL. Developmental changes of laryngeal dimensions in unparalyzed, sedated children. Anesthesiology. 2003;98(1):41-45. https://doi.org/10.1097/00000542-200301000-00010
Tucker GF, Tucker JA, Vidic B. Anatomy and development of the cricoid: serial-section whole organ study of perinatal larynges. Ann Otol Rhinol Laryngol. 1977;86(6 Pt 1):766-769. https://doi.org/10.1177/000348947708600609
Dalal PG, Murray D, Messner AH, Feng A, McAllister J, Molter D. Pediatric laryngeal dimensions: an age-based analysis. Anesth Analg. 2009;108(5):1475-1479. https://doi.org/10.1213/ane.0b013e31819d1d99
Mariyaselvam MZ, Marsh LL, Bamford S, Smith A, Wise MP, Williams DW. Endotracheal tubes and fluid aspiration: an in vitro evaluation of new cuff technologies. BMC Anesthesiol. 2017;17(1):36. https://doi.org/10.1186/s12871-017-0328-0
Gallagher TJ, Klain MM, Carlon GC. Present status of high frequency ventilation. Critical Care Medicine. 1982;10(9):613-617.
Carroll RG. Queries on cuffs. Anesthesiology. 1977;46(6):438. https://doi.org/10.1097/00000542-197706000-00016
Greaney D, Russell J, Dawkins I, Healy M. A retrospective observational study of acquired subglottic stenosis using low-pressure, high-volume cuffed endotracheal tubes. Paediatr Anaesth. 2018;28(12):1136-1141. https://doi.org/10.1111/pan.13519
Weiss M, Gerber AC, Dullenkopf A. Appropriate placement of intubation depth marks in a new cuffed paediatric tracheal tube. Br J Anaesth. 2005;94(1):80-87. https://doi.org/10.1093/bja/aeh294
Weiss M, Balmer C, Dullenkopf A, et al. Intubation depth markings allow an improved positioning of endotracheal tubes in children. Can J Anaesth. 2005;52(7):721-726. https://doi.org/10.1007/bf03016560
Jordi Ritz EM, Von Ungern-Sternberg BS, Keller K, Frei FJ, Erb TO. The impact of head position on the cuff and tube tip position of preformed oral tracheal tubes in young children. Anaesthesia. 2008;63(6):604-609. https://doi.org/10.1111/j.1365-2044.2008.05440.x
Kemper M, Imach S, Buehler PK, Thomas J, Dave M, Weiss M. Tube tip and cuff position using different strategies for placement of currently available paediatric tracheal tubes. Br J Anaesth. 2018;121(2):490-495. https://doi.org/10.1016/j.bja.2018.05.002
Moehrlen U, Ziegler U, Weiss M. Scanning electron-microscopic evaluation of cuff shoulders in pediatric tracheal tubes. Paediatr Anaesth. 2008;18(3):240-244. https://doi.org/10.1111/j.1460-9592.2007.02386.x
Peyton J, Foglia E, Lee GS. Pediatric Airway Anatomy and Tracheal Tubes: It Is Not All About the Cuff. Anesth Analg. 2021;133(4):891-893. https://doi.org/10.1213/ane.0000000000005705
Pawar D. First Do No Harm. Airway. 2020;3(1):1-3. https://doi.org/10.4103/arwy.Arwy_16_20
Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth. 2009;103(6):867-873. https://doi.org/10.1093/bja/aep290
Dariya V, Moresco L, Bruschettini M, Brion LP. Cuffed versus uncuffed endotracheal tubes for neonates. Cochrane Database Syst Rev. 2022;1(1):Cd013736. https://doi.org/10.1002/14651858.CD013736.pub2
Bernet V, Dullenkopf A, Maino P, Weiss M. Outer diameter and shape of paediatric tracheal tube cuffs at higher inflation pressures. Anaesthesia. 2005;60(11):1123-1128. https://doi.org/10.1111/j.1365-2044.2005.04359.x
Sathyamoorthy M, Lerman J, Asariparampil R, Penman AD, Lakshminrusimha S. Stridor in Neonates After Using the Microcuff® and Uncuffed Tracheal Tubes: A Retrospective Review. Anesth Analg. 2015;121(5):1321-1324. https://doi.org/10.1213/ane.0000000000000918
Higgins JPT, Thomas J, Chandler J, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons; 2019
Hansen TG, Aunsholt L, Weiss M. Ensuring the brightest start: the new European airway management guideline for neonates and infants. Eur J Anaesthesiol. 2024;41(1):1-2. https://doi.org/10.1097/eja.0000000000001908
Ponde V, Holski J, Yamashita M. Neonatal Airways and the Risks of Cuffed Tubes. JAMA Surg. 2024 Dec 4. https://doi.org/10.1001/jamasurg.2024.5185